Common Surgical Procedures for Bursitis
Reasons for Undergoing Bursa Surgery

There could be a multitude of specific reasons for a physician to recommend surgery. From a more general standpoint, the physician will try to take into account ALL factors (pain, quality of life, surgery risk, etc.) in determining whether surgery is of net benefit to you. In some cases, this is a simple determination as surgery is often performed to save a life when it is apparent the patient will die without an operation. In other cases where there is a soft tissue injury, surgery is typically the final resort option when recommended conservative treatment options have failed to help.
If you are undergoing surgery for a bursa injury, it is most likely that you have undergone a course of conservative treatments for at least a couple of months - as recommended by your doctor. They do this because it is generally understood by doctors and surgeons that surgery will introduce more scar tissue into the area. This added scar tissue will be problematic, requiring more visits to your physio clinic and conservative treatment options post-surgery. If proper recovery protocols are not undertaken following the surgery, your joint could easily wind up in worse shape than it was before the surgery! This is why surgery is only performed as a last resort.
What is the Goal of the Surgery?
Surgery is rarely undertaken unless it is has become clear that it is necessary - surgery for a soft tissue injury is a "last resort" option. The surgery performed to repair soft tissue usually involves one or more of the following surgical goals:
- Debridement - this is the removal of any loose fragments of bursa, scar tissue, bone or other debris from the area.
- Bursectomy - this is the complete removal of a bursa.
- Smoothing - the surgeon makes room so that tendons and muscles can function properly without being pinched (aka impingement). This sometimes results in shaving down of bony edges or spurs from bone so soft tissue can slide without fraying. The most common example of this in the foot would be a heel spur - a very common occurence for those suffering from plantar fasciitis.
- Stitching - torn fascia, ligament and/or tendon edges are sewn back together and reattached to the bone if needed.
- Tension Release - some individuals have shortened connective tissue (fascia, muscle and/or tendon) that can create chronic tension, putting pressure on bursae and creating strain in the connective tissue. In such cases, surgery may be undertaken to release this tension. A common example of this is plantar fasciitis - tension in the fascia can travel to the back of the heel, putting added tension on the achilles tendon and retrocalcaneal bursa. [3]
How Long To Recover From Bursitis Surgery?
Incision wounds normally take about 10 days to heal but this can depend greatly on the type of surgery that was performed (arthroscopic vs open surgery) and WHERE it was done. Most patients find significant improvement from about 4 to 6 weeks after the surgery and return to full activity from 6 to 10 weeks. [4] There are times, of course, where the area will become quite sore then go away again - this is often due to movement and stresses put on the post surgical area.
In most cases, a new bursa will grow back within a couple weeks after a bursectomy. The new bursa will most likely be healthy and will not have the pain and inflammation that may have been experienced with the removed bursa.
Why Do Recovery Rates Vary?
Everyone is different! Soft tissue recovery time after surgery depends on a multitude of factors; some include overall health, age and blood circulation levels. Further to this, some diseases may also have a substantial effect on healing times, one example being diabetes.
What Conditions May Affect My Surgery Negatively?
There are many issues, ailments and conditions that could have a negative effect on surgery outcome. Some of these would include:
- Overall health. How healthy are you? Healthy bodies are generally more capable of handling the stress of surgery.
- Diabetes, and more specifically, lack of good blood flow can lead to complications, predisposing you to many negative outcomes - even necrosis.
- Nerve disease "Sensory loss or paresthesias (uncomfortable sensations) due to nerve disease can predispose you to profound foot discomfort after surgical procedures involving your foot." [1]
Aside from the conditions listed above, surgery will typically not be undertaken if you are currently experiencing an infection in the area.
What Requirements Are Considered For Me To Be a Candidate for Bursitis Surgery?
First and foremost, you will likely only be considered for bursitis surgery after undertaking a course of conservative treatment options for at least 3 to 6 months. Other factors would likely include:
- Is Your Ability to Work Affected?
- Are You Still in Severe Pain, Despite Trying Conservative Treatment Options?
- Is This Condition Preventing You From Engaging In Physical Activity?
- Have You Been Diagnosed With Bursitis? Have Other Conditions That Exhibit Similar Symptoms Been Ruled Out?
Effective Conservative Treatment Options are Available
If you are not at the surgery stage and your physician has opted to treat your injury with conservative treatment options, then you will find that many of our customers have had great success treating themselves with the powerful conservative treatment products such as the TShellz Wrap®. When used as directed, it is our opinion that the TShellz Wrap® is a crucial part of a conservative home treatment protocol - a protocol designed to aid in the recovery process. In some cases, a dedicated approach to home conservative treatments might make enough of a difference that perhaps you will not need surgery after all. If surgical intervention is required, talk with your physician about using these same products for post-surgery recovery as they are intended to be highly effective for reducing post surgery inflammation, enhancing range of motion and minimizing scar tissue growth.
If Surgery is Required
Regardless of what type of surgery is undertaken, there are both advantages and disadvantages for each type of surgery. Once surgery is tabled as an option, speak with your physician and ensure you have a full understanding of the risks involved.
Surgery may be necessary if you have exhausted all forms conservative treatments, resting, cold, PT - and, you still find yourself in pain and have limited functionality in common daily activities. You and your doctor may decide to move forward and have you undergo surgery, triggering the next chapter of your injury recovery journey. A good point to remember is that your post surgery rehabilitation efforts will have an important impact on how soon you can return to living and enjoying your normal daily life.
If possible, avoiding surgery is typically the best option. However in some extreme cases the bursa remains thick and swollen, causing chronic bursitis pain and in such cases, a bursectomy is often advised. Surgical removal of a bursa (a procedure called a bursectomy or resection of a bursa) may be necessary if the bursa has become chronically inflamed. The type of surgery you will have depends on the type of injury you're faced with.
The surgery that your surgeon will recommend for you will depend on the level of your pain, the type of injury you have, and the amount of damage there is in the area. Damage is typically determined from your physical exams, x-rays and MRI results. The length of time between the injury and the surgery is often also a determining factor in the type of surgery that will be required.
With an acute (recent) injury, you have increased odds of qualifying for a less invasive surgery (such as arthroscopic or a mini-open procedure). Surgeons will always choose a shorter, less invasive procedure if it is possible to do so. Most surgeons know that a less complicated procedure will create less trauma to the area, resulting in a quicker rate of recovery after the surgery.
Arthroscopic Vs Open Surgery
Arthroscopic Surgery
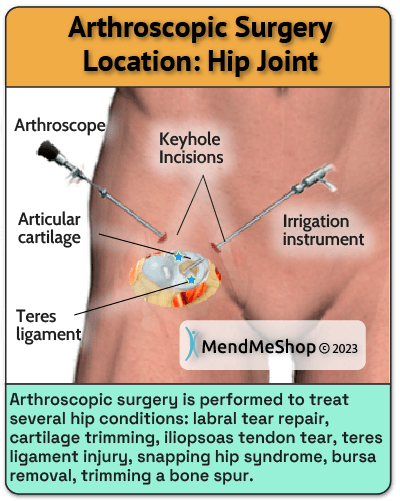
Arthroscopy can be a minimally invasive surgical procedure that is used to diagnose and/or treat some conditions. If a doctor is unable to make a diagnosis following a physical exam, x-ray, and/or MRI, an arthroscopy may be performed to get a better look inside the injury area so a diagnosis can be made.
For most soft tissue injuries, arthroscopic surgery is the preferred procedure as it is minimally invasive and patients usually recover at a much faster rate. This type of surgery will provide the surgeon with first hand insight into the nature of the injury and possibly limit the amount of soft tissue damage from surgery, helping promote a more effective recovery.
This type of surgery is also preferred when operating on joints of the body, like the shoulders or knees. Arthroscopic surgery is usually performed with the patient under general anaesthetic. During surgery, tiny incisions (1/4" - 1/3") are made to insert the surgical instruments, and a thin tube containing a camera and light.
Arthroscopic surgery will provide the surgeon with a first hand look into the nature of the injury and what work must be done to fix the injury. If the damage is not extensive, the surgeon will be able to complete the repair through an arthroscopic procedure. This is a minimally invasive procedure so it may limit the amount muscle tissue damage from surgery, helping promote a more effective recovery.
Open Surgery
Some cases however, will require open surgery as the scope of arthroscopic surgery is limited in comparison to full exposure of the bursa and surrounding tissue in open surgery. If you undergo an open surgery, you should anticipate a much longer time for rehabilitation efforts.
Traditional open surgery is used when there is substantial damage in the area and/or the surgeon needs to physically open up the area to better assess the damage. This could include damage to one or more of the following: muscle, bursae, tendon, cartilage, ligaments, fascia and/or bone fractures. During this procedure a sizable incision is made in the area of the injury.
An Overview of Commonly Used Surgical Solutions for Bursitis
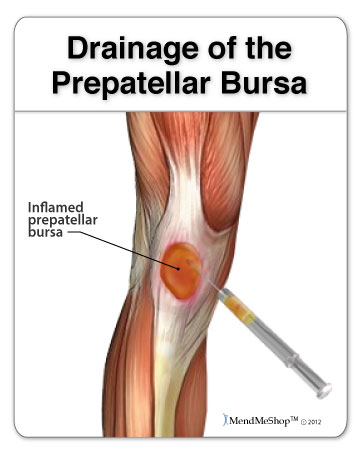
Bursa Draining, Bursa Aspiration
Generally when it comes to bursitis surgery you'll be faced with options for non-invasive procedures or more invasive solutions. If it's possible to do a non-invasive procedure, your doctor may suggest a less aggressive procedure such as draining or aspiration of your enlarged bursa.
The hope is that the removal of extra fluid from your bursa will reduce your pain, but it may only be a temporary fix if the bursa sac has thickened walls and has chronic inflammation. The cause of fluid build-up will also require treatment with conservative treatment methods following the procedure.
Bursitis Aspiration Surgery
This procedure is most commonly used for elbow bursitis. Your doctor will use a syringe filled with liquid (1% lidocaine) to raise the skin over the bursa and to freeze/numb the area. Your doctor raises the tissue to protect the tendons and ligaments in the elbow. A new needle will then be inserted into the bursa to drain the fluid and reduce the overall size.
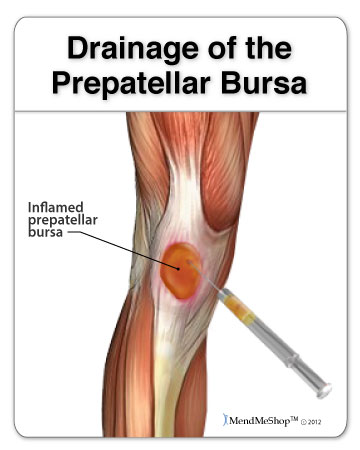
Joint Arthrocentesis Surgery
Your doctor will insert a needle into the bursa and drain the fluid. This type of joint aspiration is common for treating bursitis in the knee, wrist, hip or shoulder. This type of procedure is used to protect the joint from further (more invasive) surgery and a more complicated outcome.
Once you've had your bursa drained of the extra fluid, the pressure on your surrounding soft tissue (ligaments, tendons, muscle) should be reduced. Even though this procedure may ease your pain, you'll still need to rest the injury and continue with conservative treatment methods for post-surgery recovery. Your doctor will encourage you to use a Cold Compress or Ice Pack at the start to get the swelling down, then eventually progress to stretching/exercise, home treatments such as the TShellz Wrap® and most importantly - rest.
Draining extra fluid from the bursa isn't considered a cure for the bursitis injury. Your bursa might re-fill with fluid and the risk of re-injury is still quite high. If you find that your bursitis has come back and you're suffering even more than before, you may need to have the bursa removed from the joint.
Bursa Removal Surgery (aka "Bursectomy")
The bursectomy, a surgery performed to remove a problematic bursa, has become more common than in the past. Only a doctor will be able to make a proper diagnosis to determine if surgery is necessary and/or recommend for your bursa. An MRI or x-ray may be necessary for an accurate diagnosis. An x-ray will show if the problem could be bone related, and an MRI produces an image of the muscles, tendons, bursae and ligaments that may be damaged or displaced. As you may know, bursitis and tendonitis occur very commonly together, and if there is both tendon and bursa damage, the MRI results signify as much. The MRI results are important as both surgery and the type of surgery undertaken (open surgery vs arthroscopic) will depend on whether there is only bursa damage or if there is tendon, ligament and/or muscle damage as well.

Open Bursitis Surgery (Bursectomy)
Traditional open surgery is used when there's a large amount of damage to the bursa tissue, bone fractures in the joint as a result from an acute injury, bone spurs or other injuries from degeneration (aging) of your joint and/or extensive damage to the surrounding soft tissue (tendons, ligaments, muscle). During this procedure one long incision(s) is made in the area of your injury. An open incision this large provides enough room for the surgeon to remove the bursa, shave down any bone spurs and repair any damaged tissue. Open surgery is rarely used except in some cases of knee and shoulder bursitis.
An open procedure is rarely used for elbow bursitis (only the most extreme cases). In some cases, an open procedure will also be used for larger, more involved hip bursitis removal. However if it's possible to do so, a surgeon will usually remove one or more of the bursae in the hip with arthroscopic surgery.
An open procedure with precise suturing of soft tissue improves overall strength in the joint during the recovery process, making recovery setbacks less likely.
Arthroscopic Bursitis Surgery (Bursectomy)
A bursectomy will be done arthroscopically if your damaged bursa is accessible through 2 to 4 keyhole incisions in your joint. This type of procedure is common for shoulder (subacromial) bursitis, knee (prepatellar, infrapatellar, pes anserine) bursitis, and hip (iliopsoas, trochanteric) bursitis.
Arthroscopic bursitis surgery will provide the surgeon with a first hand look into the nature of the injury and what work must be done to remove your bursa. During this procedure a thin tube containing a camera and light is inserted through an incision near the joint. Additional surgical tools required to remove/fix your bursa will be inserted into the other keyhole incisions. A shaver is sometimes used to cut the bursa free from the surrounding tissue and then the bursa will be removed. If a bone spur or other problem has caused the bursitis, the spur is removed or the problem is corrected to prevent further issues.
This is a minimally invasive procedure so it may limit the amount of tissue damage from surgery, helping promote a more effective recovery. Your surgeon will preform bursectomy surgery with the goal to have you on the road to recovery faster. Rehabilitation from a bursectomy will depend on your healing ability, rest, your diet, tissue damage, and other procedures done during the surgery.
Generally, recovery time is relatively fast (6 weeks to 12 weeks) after a bursectomy as long as post surgery recovery protocols are adhered to.
Debulking or Debridement
This surgical technique is done during open surgery and is undertaken when there is scar tissue, bone spurs, and/or a lot of soft tissue damage in the joint. To perform a debulking or debridement the surgeon will cut away any damaged/inflamed tissue. If muscle or tendon soft tissue is torn or ruptured, they will also scrape down any calcium deposits (bone spurs) that have formed on the bone. Scar tissue may be removed from the muscle fibers, tendons, tendon sheath surrounding the tissue or from both surfaces.

Joint Specific Surgery Details
Wrist Bursitis Surgery & Recovery
Your surgeon will start with a less aggressive approach to deal with your wrist bursitis first. This is done to avoid open surgery to remove the bursa from your wrist. Usually an arthrocentesis procedure is used to treat wrist bursitis. This is where a needle is inserted into the bursa to drain the fluid. If you're suffering from chronic wrist bursitis your doctor may decide to have you undergo an arthroscopic surgery to remove the bursa sac altogether. No matter what type of procedure you have for your wrist, you'll need to wear a splint on your wrist for 1 to 2 weeks after the surgery. You'll also need to limit weight bearing and lifting of the affected hand and wrist.

Foot Bursitis Surgery & Recovery
Bursae in the foot are known as adventures. This means that your body will create some bursae in the foot in response to damage to the foot (to help compensate for other soft tissue injuries in the foot).
Some of the places where "adventure" bursae will grow in the foot include:
- the first metatarsal phalangeal joint (the base of the big toe), often associated with a bunion and Morton's Neuroma
- the base of the second metatarsal phalangeal joint (the base of the second toe)
- the base of the fifth toe, often associated with a bunionette
- the bottom of the heel and the bottom of the forefoot
- the ankle area
Metatarsal bursa and inter-metatarsal bursitis injuries respond best to conservative treatments (rest, application of a Cold Compress or Ice Pack, Circulation Boost via a TShellz Wrap® and a good stretching routine).
Visits to the PT clinic will focus on restoring the correct position of bones and soft tissue in the foot. Your doctor won't consider surgery without you first trying conservative treatment methods and correcting the mechanics of your foot in PT. Shoe modification with an orthotic may be the only treatment required, although in severe cases, surgical realignment of the metatarsal bones may be required.
Foot surgery is only considered as a last resort option. Why? Scar tissue in the foot will cause more problems to the soft tissue in your foot, possible moreso than the original bursa injury. Surgical techniques are always improving, but post-surgical complications arising from foot surgery are not infrequent and can have a huge impact on quality of life.
Achilles (Ankle or Heel) Bursitis Surgery & Recovery

Achilles/ankle/heel bursitis (retrocalcaneal bursitis), also known as Haglund's Syndrome, can only be treated through open surgery. The medical community has not come up with the most effective type of surgery to deal with the Retrocalcaneal Bursa. What is known is there are two different approaches to solving retrocalcaneal bursa pain. [2]
1. Open surgery with the removal of the retrocalcaneal bursa.
The surgeon may or may not carefully cut away any dead tissue in the Achilles tendon and shave down the calcaneal bone. After the surgery you'll be placed in a short leg cast for 2 weeks with your ankle in a flexed down position. Then you'll be placed in a neutral ankle position for another 2 weeks. To protect the tissue while healing you won't be allowed to bear any weight on your ankle and take part in activities that place weight on your ankle for the first 4 weeks following surgery.
Approximately 6 weeks after surgery, you'll be placed in a walking boot for another 2 weeks. It will be important to stick to your clinic appointments and continue exercise at home during your entire recovery process. Complete recovery time for heel bursitis surgery is between 6 months and 2 years.
2. Open surgery by splitting the Achilles tendon to allow access to drain the bursa, cut away dead tissue on the bursa sac or completely remove the bursa.
This tendon-splitting approach has some major drawbacks because it weakens the Achilles tendon and the recovery process to return to full function of the foot is very slow. A build-up of scar tissue may cause more irritation to the foot after recovery, possibly requiring additional conservative treatment methods or even more surgery.
Elbow (Olecranon) Bursitis Surgery & Recovery

The elbow has very poor blood supply and may not heal correctly after open surgery. A build up of scar tissue in the elbow can affect range of motion later on so your doctor/surgeon may opt to use this less invasive procedure for your elbow bursitis...
If your condition is chronic, a small incision will be made over the bursa. Surgery is only done when the bursa is not red, hot, and inflamed. If the bursa has become thickened and enlarged this procedure will involve lifting the skin on your elbow up, over the swelling. If this is the case, there will be a considerable empty 'dead space' left behind where the enlarged bursa once was. This space often fills with blood and fluid after the operation. Your surgeon will apply a firm bandage to reduce the amount of fluid that collects. You may need to visit the doctor to have additional fluid drained from your elbow with a syringe.
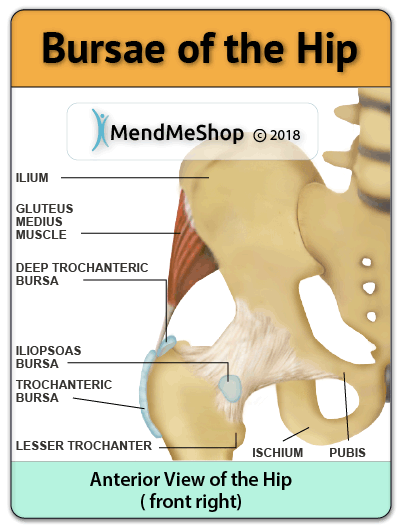
Hip (Trochanteric / Iliopsoas) Bursitis Surgery & Recovery
During this procedure your surgeon will make 2 to 3 small incisions in and around your hip. Your surgeon will insert small tools into the hip joint to repair, remove and/or shave your damaged bursa tissue. If trochanteric surgery is being performed, the surgical team will apply pressure to your hip to help open up the area allowing your surgeon access to tissue. If you're suffering from a secondary condition along with bursitis, your surgeon may need to add 1 to 2 more incisions for additional soft tissue repair.
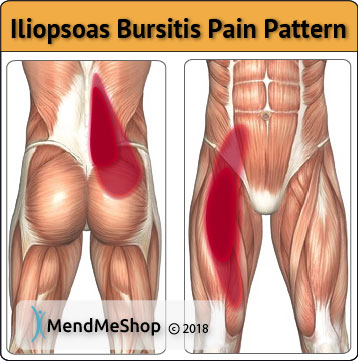
If one of the tendons in your hip need to be cut to allow your bursa to be removed, this tendon may also be lengthened or released (cut) to give your bursa more room in the hip joint. If the tendon is not repaired, the edges will heal and fill in with scar tissue. The tendon will end up being much looser than before you had surgery. Generally, the surgeon wants to make sure your greater trochanter tissue isn't rubbing on the surface of the other tissue in your hip.
During post-operative recovery from hip bursitis surgery you'll be on crutches for 2 to 4 weeks. You'll also need to wear a brace for 2 weeks to protect the delicate tissues in your hip and prevent extreme movement. The brace will need to be worn over your clothing during weight bearing activities while still using your crutches. You may also need to wear the brace while you sleep for the first week after surgery.
Recovering from hip bursitis surgery is a slow process. You'll have to attend PT sessions quite a few times a week during your post-surgery recovery for a period that may take several months. You'll be encouraged to move around as soon as possible, but with care placed on protecting your hip and the tissues as they heal.
During physio you can expect to experience proactive range-of-motion exercises and work your way up to active stretching and strengthening of the muscles and tendons in your hip, thigh and leg. This will most likely include riding a stationary bike 2 times a day, every day, for 5 to 10 minutes.
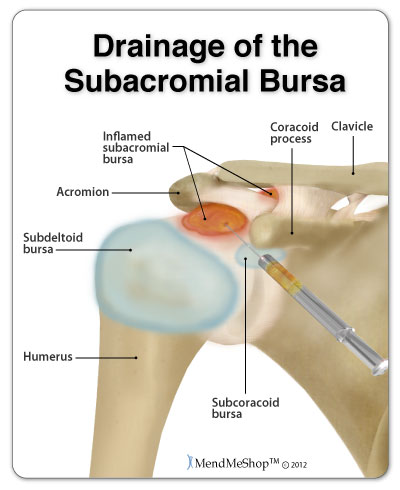
Shoulder (Subacromial) Bursitis Surgery & Recovery

Shoulder bursitis can be surgically treated with an arthroscopic procedure, using a small camera to see your shoulder joint. Your surgeon will make 2 keyhole incisions at the front of your shoulder. Small instruments will then be inserted into the the shoulder joint. Your surgeon will use these tools to see any tears, bone spurs or loose material, and remove or shaving away dead tissue on your damaged bursa sac (this is also called debridement).
During your initial recovery from surgery you'll have to protect your shoulder and arm by wearing a sling or splint. You'll be encouraged to do normal daily activities, raising your arm waist high, after a few days. Attending physio appointments will help with range of motion, stiffness and swelling. Recovery for shoulder bursitis surgery is usually between 2 to 6 months depending on the amount of work your surgeon had to do to repair / remove the bursa sac in your shoulder.
Knee Bursitis Surgery & Recovery
(Prepatellar, Infrapatellar, Pes Anserine)
If your bursa needs to be removed your surgeon will make an incision into the skin over the length of your bursa. The surgeon will use care to remove the bursa from the surrounding tissue to make sure they don't tear or rupture the bursa itself. Once the bursa is removed the surgeon will use strong 'mattress' sutures on your inner soft tissue and the skin to close the opening. Mattress sutures are used to help fill in the gap ('dead space') left from the bursa that's been removed. These sutures also allow the surgeon to apply tension to the inner tissue and reduce the build-up of scar tissue inside the joint.
Post-operative care after a knee bursectomy (removal of the bursa) will begin with a large compression dressing that's applied to your knee. Your whole leg, from groin to ankle, will be completely immobilized for 2 weeks until the wound from surgery is completely healed. Your surgeon may have you start quadricep exercises the day after surgery, this depends on the amount of repair required during the surgery.
Another option for surgery is drainage of the bursa in your knee. After this procedure your knee and leg will need to be immobilized in a splint. If your surgeon has used gauze to catch any additional fluid that leaks, this gauze dressing will need to be changed at least twice a week. There will now be some 'dead space' left inside of your knee where the bursa fluid once was. As your body tries to heal the area, even more fluid may collect inside this space in your knee joint. If this happens your surgeon will tell you to continue immobilizing your leg and knee to reduce the build up of fluid.
Stability of your Joint after Bursa Surgery
It is important to understand that surgery may not give you 100% functionality of your joint, but you should be able to return to most if not all of your pre-injury activities. Surgical procedures (outlined above) are often performed with very successful results. What truly makes a difference is your commitment to a doctor recommended rehabilitation program after surgery as there is always a possibility of re-injury even after a surgical procedure. One complication of surgical repair for muscle/tendon tear is that skin can become thin at site of incision, and may have limited blood flow.
Ask any doctor and they will tell you that the success of your surgery depends on your level of dedication to your recovery. Most of our bursitis post-op clients have experienced positive results through adhering to a dedicated home conservative treatment regiment involving regular use of a Cold Compress or Ice Pack, a TShellz Wrap® and a stretching program as recommended by their physician.
FREE SHIPPING ON ALL PRODUCTS CURRENTLY ENABLED
Product specialists are available 9:00 am to 5:00 pm Eastern Standard Time Monday to Friday.
If any question or concern arises, call us or simply send us an email at any time (we check our emails constantly all throughout the day and night.. even on holidays!). We will respond as soon as possible.
North America Toll Free 1-866-237-9608
Outside North America +1-705-532-1671
Please be aware that this information is neither intended nor implied to be a substitute for professional medical advice. All testimonials and comments reflect the real life experiences of individuals that used our products, however, individual results may vary. Always seek the advice of your physician or other qualified health provider before using any of our outstanding products to make sure they are right for you and your condition or if you have any questions regarding a medical condition.
For more information, call us via: 1-866-237-9608 or send us an email. View our Privacy Policy.
The terms Inferno Wrap®, Freezie Wrap®, T-Shellz® and Mendmeshop.com® are registered trademarks of In.Genu Design Group Inc.
All images shown are exclusive Copyright© 2006 - 2025 AidMyBursa.com.
Sources:
1. "Trochanteric Bursitis Surgery Sydney NSW | Hip Injury Treatment Darlinghurst." Hipandkneesurgery.com.au. N. p., 2018. Web. 18 Oct. 2018.
2. Anderson JA, Suero E, O'Loughlin PF, Kennedy JG. Surgery for retrocalcaneal bursitis: a tendon-splitting versus a lateral approach. Clin Orthop Relat Res. 2008 Jul;466(7):1678-82. doi: 10.1007/s11999-008-0281-9. Epub 2008 May 9. PMID: 18465183; PMCID: PMC2505264.
3. Plantar Fasciitis. The. (2023) Plantar Fascia Release: Preparation, Recovery, Long-Term Care. Retrieved April 04, 2023, from https://www.verywellhealth.com/surgery-for-plantar-fasciitis-2549873
4. (2023) Bursitis/ Impingement Surgery | Rothman Orthopaedic Institute. Retrieved May 17, 2023, from https://rothmanortho.com/specialties/treatments/bursitis-impingement-surgery